Teen Mental Health Crisis & Therapy Waitlists: A Comprehensive Guide to Understanding, Overcoming, and Supporting Our Youth
Teen Mental Health Crisis & Therapy Waitlists: A Comprehensive Guide to Understanding, Overcoming, and Supporting Our Youth
Table of Contents
- Understanding the Teen Mental Health Crisis
- The Therapy Waitlist Problem: A Critical Barrier
- Impact of Treatment Delays on Adolescent Development
- Waitlist Management Strategies That Work
- Supporting Teens While Waiting for Treatment
- Innovative Solutions and Alternative Approaches
- Guidance for Families and Caregivers
- Policy Recommendations and System Changes
- Frequently Asked Questions
- Conclusion and Call to Action

Understanding the Teen Mental Health Crisis
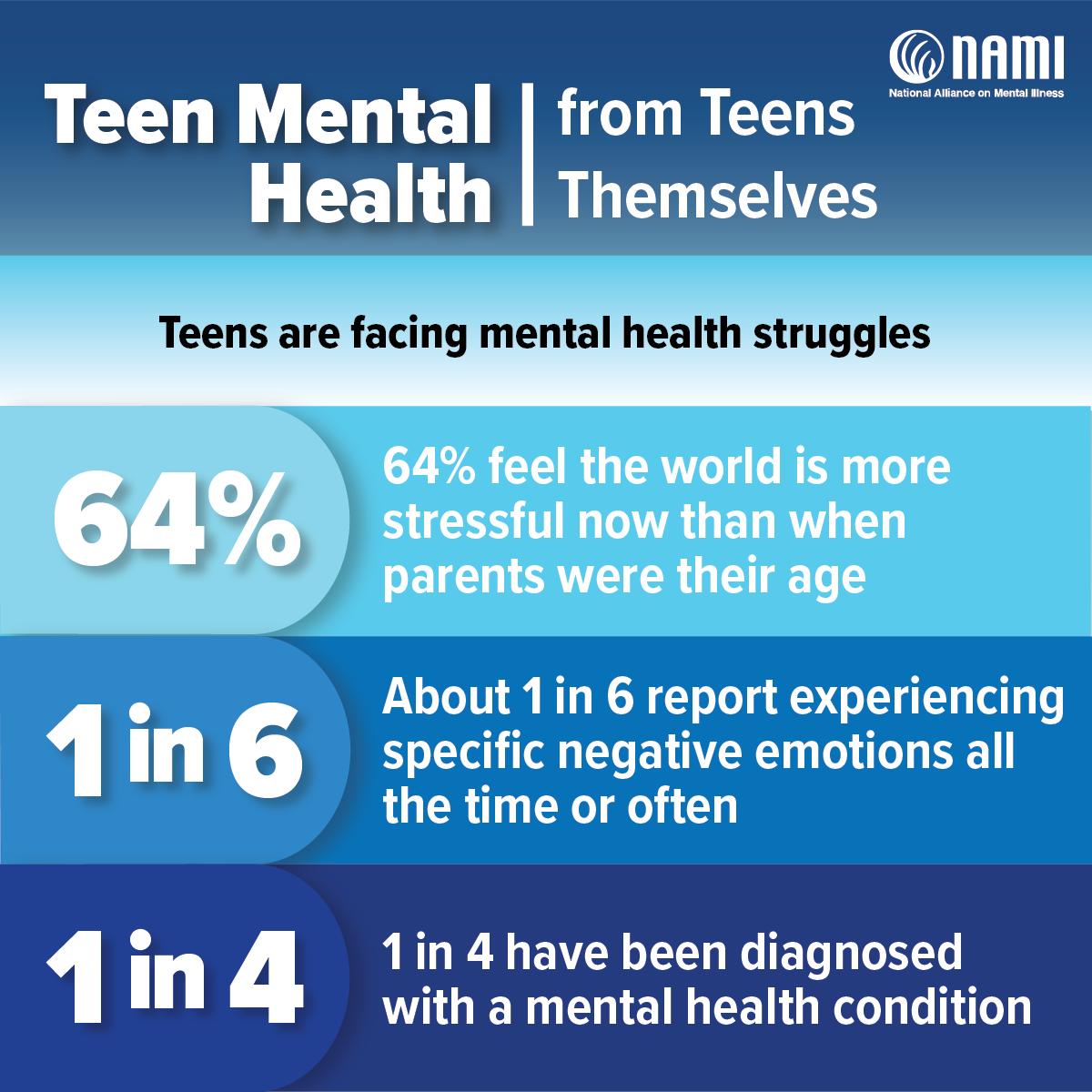
The adolescent mental health crisis represents one of the most pressing public health challenges of our time. Current data reveals that 25.2% of adolescents experience anxiety symptoms and 20.5% face depression symptoms – rates that have doubled since before the COVID-19 pandemic. This surge in mental health difficulties coincides with a critical developmental period where the peak age of onset for most mental disorders is 14.5 years.
Mental health disorders including anxiety, depression, attention-deficit/hyperactivity disorder (ADHD), and conduct problems adversely impact 13-22% of children and adolescents in North America, creating a significant burden on both individuals and healthcare systems. The ripple effects extend far beyond the immediate symptoms, influencing academic performance, social relationships, family dynamics, and long-term life outcomes.
Key Drivers of the Mental Health Crisis
Mental health professionals surveyed across all 50 states have identified three primary drivers of the current crisis:
- Social Media Impact: Increased social comparisons, FOMO (fear of missing out), and cyberbullying
- Social Isolation: Reduced face-to-face interactions and community connections
- External Stressors: School shootings, climate change, political instability, and global uncertainty
Additional contributing factors include lack of independence skills, missed developmental milestones due to pandemic disruptions, perfectionism pressures, and family instability. These interconnected challenges create a perfect storm that overwhelms many adolescents' coping mechanisms.
The Therapy Waitlist Problem: A Critical Barrier
While the need for mental health services has skyrocketed, access remains severely limited. The most significant barrier facing families seeking help is the extensive waitlist system that has developed across mental health services. Survey data from clinicians reveals that "waitlists tend to be 6-12 months to get into services," with some areas experiencing even longer delays.

The Numbers Behind the Crisis
Recent research highlights the severity of the access problem:
- More than half of the U.S. population lives in areas with mental health professional shortages
- Non-attendance rates for initial appointments can reach 15-36% when wait times exceed 30 weeks
- Nearly 50% of families contact multiple agencies after being placed on a waitlist, artificially inflating demand
- Rural areas are disproportionately affected, with some regions having virtually no youth mental health resources
Regional Disparities and Access Challenges
The waitlist crisis isn't uniform across all areas. Rural communities face particularly acute shortages, with clinicians reporting: "Rural areas around us have little to no resources" and "There is a shortage of people who can treat children, especially under age 10." Urban areas, while having more providers, still struggle with overwhelming demand that far exceeds capacity.
Impact of Treatment Delays on Adolescent Development
The consequences of delayed mental health treatment extend far beyond temporary discomfort. Research demonstrates that lengthy wait times can:
Worsen Mental Health Outcomes
- Symptom Escalation: Untreated anxiety often progresses to depression, creating more complex treatment needs
- Increased Severity: Conditions that could be managed with early intervention often require more intensive treatment after delays
- Reduced Treatment Engagement: Patients who wait longer show decreased motivation and engagement once services become available
- Lower Treatment Satisfaction: Extended wait times correlate with poorer treatment outcomes and reduced patient satisfaction
Broader Life Impact
Beyond clinical symptoms, treatment delays affect multiple life domains:
- Academic Performance: Untreated mental health issues significantly impact school achievement and graduation rates
- Social Development: Peer relationships and social skills development suffer during prolonged periods without support
- Family Stress: Caregivers experience significant burden managing children with untreated mental health needs
- Emergency Services Usage: Delayed treatment often leads to costly emergency room visits and crisis interventions
Waitlist Management Strategies That Work
Mental health systems worldwide have developed innovative approaches to address the waitlist crisis. Research has identified five broad categories of effective strategies:
1. Walk-in and Same-Day Access Models
These approaches eliminate traditional appointment scheduling by offering immediate access options:
- Open Access Scheduling: Reserved slots for same-day appointments
- Crisis Walk-in Hours: Designated times when teens can receive immediate assessment
- Flexible Scheduling: Adaptable appointment systems that respond to urgent needs
2. Enhanced Triage and Prioritization Systems
Sophisticated triage systems ensure that the most urgent cases receive priority attention:
- Risk Assessment Protocols: Standardized tools to identify high-risk patients
- Severity-Based Prioritization: Matching urgency levels with appropriate wait times
- Regular Re-assessment: Ongoing monitoring of patients on waitlists to catch deterioration
3. Multidisciplinary Care Teams
Expanding the range of professionals who can provide mental health support:
- Integrated Care Models: Combining mental health with primary care services
- Peer Support Programs: Training teens with lived experience to support others
- School-Based Services: Bringing mental health professionals into educational settings
4. Patient-Led and Self-Management Approaches
Empowering teens and families to take active roles in their mental health journey:
- Digital Mental Health Tools: Apps and online resources for self-guided support
- Psychoeducation Programs: Teaching teens and families about mental health management
- Peer-to-Peer Support Groups: Facilitated group experiences while waiting for individual therapy
5. Service Delivery Innovations
Reimagining how mental health services are provided:
- Telehealth Expansion: Remote therapy options that increase access and reduce barriers
- Intensive Short-Term Interventions: Concentrated treatment models that achieve results faster
- Group Therapy Options: Efficient delivery models that serve multiple patients simultaneously
Supporting Teens While Waiting for Treatment
While working to access professional help, families can implement evidence-based strategies to support their teen's mental health:
Immediate Support Strategies
- Crisis Resources: Ensure teens know how to access the National Suicide & Crisis Lifeline (988) or Crisis Text Line (Text HOME to 741741)
- Safety Planning: Work with teens to identify warning signs and coping strategies
- Routine Maintenance: Maintain consistent sleep, exercise, and nutrition patterns
- Social Connection: Facilitate safe social interactions with trusted peers and family members
Skill-Building Activities
Help teens develop coping skills that will benefit them regardless of when formal treatment begins:
- Mindfulness and Meditation: Apps like Headspace for Teens or Calm offer guided practices
- Journaling: Regular writing can help teens process emotions and identify patterns
- Physical Activity: Regular exercise significantly impacts mood and anxiety levels
- Creative Outlets: Art, music, and other creative activities provide emotional expression opportunities
Family Support Systems
Parents and caregivers play crucial roles in supporting teens during the waiting period:
- Active Listening: Create safe spaces for teens to express their feelings without judgment
- Validation: Acknowledge the reality of their struggles while maintaining hope
- Advocacy: Continue pursuing multiple avenues for professional help
- Self-Care: Maintain parental mental health to better support the teen
Innovative Solutions and Alternative Approaches
Forward-thinking communities and healthcare systems are implementing creative solutions to address the waitlist crisis:
Technology-Enhanced Care
- AI-Powered Triage: Automated systems that help prioritize cases and match teens with appropriate resources
- Virtual Reality Therapy: Immersive treatment options for anxiety and trauma-related conditions
- Chatbot Support: 24/7 available digital companions trained in crisis intervention
Community-Based Innovations
- Youth Mental Health First Aid: Training community members to provide initial support and referrals
- Peer Navigator Programs: Young adults with lived experience helping teens navigate the mental health system
- Mobile Crisis Teams: Rapid response units that provide immediate assessment and support
Educational System Integration
- Mental Health Curriculum: Incorporating emotional wellness education into standard curriculum
- Early Warning Systems: Using academic and behavioral data to identify at-risk students
- Embedded Clinicians: Placing mental health professionals directly in schools for immediate access
Guidance for Families and Caregivers
Navigating the mental health system while supporting a struggling teen requires specific strategies and knowledge:
Advocating Effectively
- Document Everything: Keep detailed records of symptoms, incidents, and attempts to access care
- Know Your Rights: Understand insurance coverage and appeal processes
- Build Relationships: Develop connections with school counselors, pediatricians, and community resources
- Be Persistent: Continue contacting multiple providers and check for cancellations regularly
Managing the Waiting Period
- Set Realistic Expectations: Prepare teens for potential wait times while maintaining hope
- Create Structure: Maintain predictable routines that provide stability
- Monitor Closely: Watch for changes in symptoms that might require immediate intervention
- Celebrate Small Wins: Acknowledge progress and positive coping efforts
Financial Considerations
Mental health treatment costs can be overwhelming, but options exist:
- Insurance Navigation: Understand coverage limitations and appeal processes
- Sliding Scale Options: Many providers offer reduced fees based on income
- Community Resources: Local organizations often provide free or low-cost services
- Employee Assistance Programs: Many employers offer mental health benefits for employees and family members
Policy Recommendations and System Changes
Addressing the teen mental health crisis and waitlist problems requires coordinated policy efforts at multiple levels:
Healthcare System Reforms
- Insurance Parity Enforcement: Ensuring mental health coverage equals physical health coverage
- Reimbursement Rate Improvements: Increasing payment rates to attract more providers to accept insurance
- Workforce Development: Expanding training programs for child and adolescent mental health specialists
- Integration Incentives: Promoting collaboration between mental health and primary care providers
Educational Policy Changes
- Mandatory Mental Health Education: Including social-emotional learning in curriculum standards
- Counselor-to-Student Ratios: Establishing and funding appropriate staffing levels
- Early Identification Systems: Implementing screening and referral protocols in schools
- Crisis Response Protocols: Developing comprehensive emergency response plans for mental health crises
Community Investment Priorities
- Youth Mental Health Hubs: Creating centralized locations for comprehensive services
- Public Awareness Campaigns: Reducing stigma and promoting help-seeking behavior
- Crisis Infrastructure: Developing alternatives to emergency rooms for mental health crises
- Prevention Programs: Investing in upstream interventions that prevent mental health problems
Frequently Asked Questions
How long should I expect to wait for teen mental health services?
Wait times vary significantly by location and provider type, but surveys indicate 6-12 months is common for many areas. Urban areas may have shorter waits but higher demand, while rural areas often have limited options. Contact multiple providers simultaneously and ask to be placed on cancellation lists to reduce wait times.
What should I do if my teen is in crisis while on a waitlist?
If your teen is experiencing suicidal thoughts, self-harm, or severe symptoms, don't wait for scheduled appointments. Contact the National Suicide & Crisis Lifeline at 988, go to your nearest emergency room, or call 911. Many areas also have mobile crisis teams that can provide immediate support.
Can schools provide mental health support while we wait for outside services?
Many schools have counselors, social workers, or psychologists who can provide support, crisis intervention, and referrals. However, school resources are often limited. Contact your teen's guidance counselor or school mental health professional to discuss available options and support strategies.
Are there effective online or app-based resources for teens waiting for therapy?
Yes, several evidence-based digital tools can provide support while waiting. Options include Crisis Text Line (text HOME to 741741), apps like Headspace for Teens, and online therapy platforms. However, these should supplement, not replace, professional care for teens with significant mental health needs.
How can I tell if the wait is affecting my teen's mental health?
Warning signs that the wait is harmful include worsening symptoms, increased hopelessness, social withdrawal, declining academic performance, or expressions of self-harm. If you notice deterioration, contact your teen's primary care provider, reach out to crisis services, or consider emergency intervention.
What insurance issues should I be aware of when seeking teen mental health care?
Common issues include limited provider networks, prior authorization requirements, session limits, and low reimbursement rates that cause providers to not accept insurance. Review your coverage carefully, understand appeal processes, and ask providers about payment options if insurance coverage is inadequate.
Conclusion and Call to Action
The teen mental health crisis, compounded by extensive therapy waitlists, represents a critical challenge that demands immediate, coordinated action from families, healthcare providers, educators, and policymakers. While the statistics are sobering – with 25% of teens experiencing anxiety and 20% facing depression – there are evidence-based strategies and innovative solutions that can make a meaningful difference.
The key to addressing this crisis lies in multiple parallel approaches: improving access to immediate care, supporting teens and families during waiting periods, implementing systemic changes to reduce barriers, and investing in prevention and early intervention programs. Every stakeholder has a role to play in creating a mental health system that truly serves our youth.
Immediate Steps You Can Take
- For Parents: Don't wait for a crisis – seek help early, document your teen's needs, and advocate persistently for services
- For Educators: Learn to recognize mental health warning signs and connect families with appropriate resources
- For Healthcare Providers: Implement waitlist management strategies and consider innovative service delivery models
- For Policymakers: Prioritize mental health funding, workforce development, and insurance parity enforcement
- For Communities: Support local mental health organizations and advocate for youth-friendly services
The teen mental health crisis and therapy waitlist problem are solvable challenges, but they require sustained effort, adequate resources, and genuine commitment to prioritizing youth mental health. By working together and implementing the strategies outlined in this guide, we can build a future where every teenager has timely access to the mental health support they need and deserve.
Remember: If you or a teen you know is in crisis, don't wait. Contact the National Suicide & Crisis Lifeline at 988 or text HOME to 741741 for immediate support.
Take Action Today
Share this resource with other families, educators, and community members. Advocate for improved mental health services in your area. Most importantly, prioritize the mental health conversations with the teens in your life – early intervention and open communication can make all the difference.
