Mpox: Complete Guide to Symptoms, Prevention, and Treatment in 2025
Mpox: Complete Guide to Symptoms, Prevention, and Treatment in 2025
Mpox, formerly known as monkeypox, continues to be a significant public health concern worldwide. This viral disease, which gained global attention during the 2022 outbreak, affects thousands of people annually and requires comprehensive understanding for effective prevention and management. This complete guide covers everything you need to know about mpox in 2025.
What is Mpox?
Mpox is an infectious viral disease caused by the monkeypox virus, a member of the Orthopoxvirus genus. This family includes the viruses that cause smallpox, cowpox, and vaccinia. First identified in laboratory monkeys in 1958, the first human case was documented in 1970 in the Democratic Republic of the Congo.
The virus exists in two main clades: Clade I (historically found in Central Africa) and Clade II (found in West Africa). Clade I is generally associated with more severe disease and higher mortality rates, while Clade II caused the 2022 global outbreak with significantly lower fatality rates.
Key Characteristics
- Double-stranded DNA virus in the poxvirus family
- Natural reservoir believed to be small mammals in tropical Africa
- Can infect both humans and animals
- Most people recover completely within 2-4 weeks
Recognizing Mpox Symptoms
Mpox symptoms typically appear 1-21 days after exposure, with most people developing symptoms within a week. The disease progresses through distinct stages, making early recognition crucial for preventing spread.

Early Symptoms (Prodrome Phase)
- Fever and chills
- Headache and muscle aches
- Back pain and low energy
- Swollen lymph nodes (distinctive feature)
- Sore throat
Rash Development
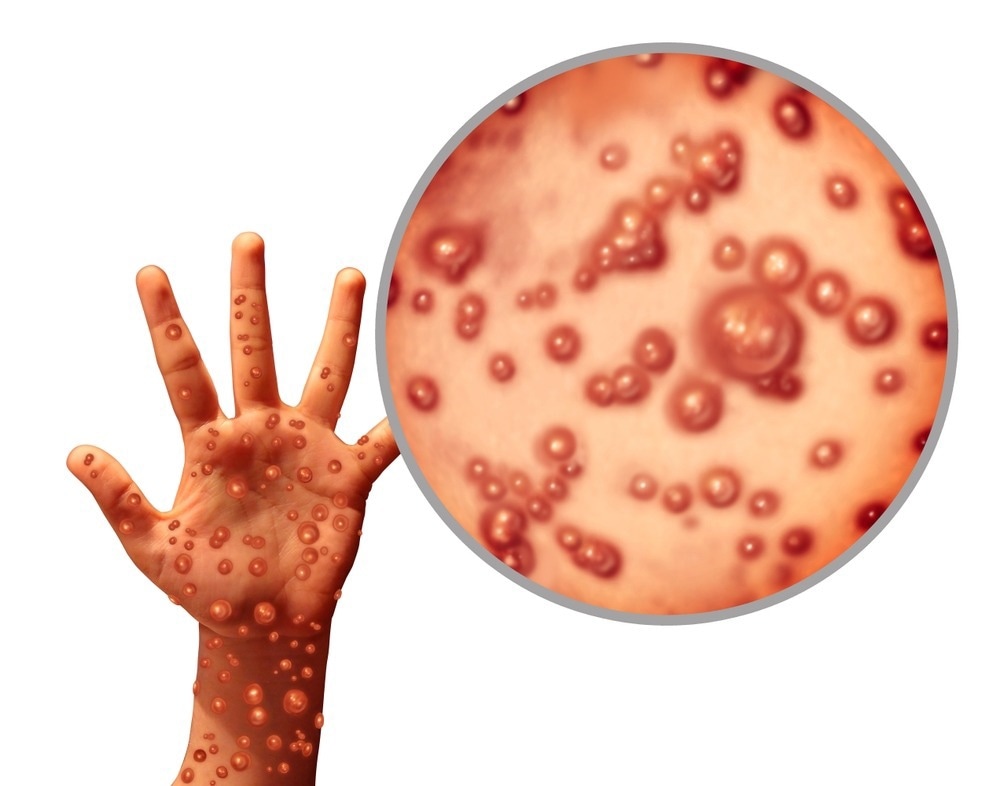
The characteristic mpox rash typically appears 1-3 days after fever onset, progressing through several stages:
- Macules: Flat, discolored spots
- Papules: Raised bumps
- Vesicles: Fluid-filled blisters
- Pustules: Pus-filled lesions
- Scabs: Crusted lesions that eventually fall off
The rash can appear anywhere on the body, including face, palms, soles, genitals, and inside the mouth. During the 2022 outbreak, many cases presented with rash only in the genital or anal areas.
How Mpox Spreads
Understanding transmission routes is essential for effective prevention. Mpox spreads through multiple pathways:
Human-to-Human Transmission
- Direct contact: Touching rash, scabs, or body fluids
- Respiratory droplets: Prolonged face-to-face contact
- Sexual contact: Close intimate contact during sex
- Contaminated materials: Clothing, bedding, towels
Animal-to-Human Transmission
- Bites or scratches from infected animals
- Handling infected animal products
- Consuming inadequately cooked meat from infected animals

Diagnosis and Testing
Accurate diagnosis requires laboratory confirmation, as mpox can be confused with other conditions like chickenpox, measles, or bacterial skin infections.
Diagnostic Methods
- PCR Testing: Gold standard using samples from lesions
- Viral DNA Detection: Swabs from rash, throat, or anus
- Clinical Assessment: Symptom evaluation and exposure history
Healthcare providers should consider mpox in patients presenting with characteristic rash, especially those with recent travel to endemic areas or close contact with confirmed cases.
Prevention Strategies
Prevention combines vaccination, behavioral modifications, and public health measures.
Vaccination
Several vaccines are available for mpox prevention:
- Jynneos (MVA-BN): Preferred vaccine, two doses given 28 days apart
- ACAM2000: Single dose, not recommended for immunocompromised individuals
Vaccination is recommended for high-risk groups including:
- Healthcare workers treating mpox patients
- Laboratory personnel handling specimens
- Individuals with multiple sexual partners
- People with recent high-risk exposures

General Prevention Measures
- Avoid close contact with people who have rash illness
- Practice safe sex and use barrier protection
- Maintain good hand hygiene
- Avoid sharing personal items like clothing or bedding
- Stay home when experiencing symptoms
Treatment Options
Most mpox cases resolve without specific treatment, but supportive care and antivirals may be used for severe cases.
Supportive Care
- Pain management with over-the-counter medications
- Maintaining hydration and nutrition
- Preventing secondary bacterial infections
- Isolation until all lesions heal
Antiviral Medications
- Tecovirimat (TPOXX): FDA-approved for severe cases
- Brincidofovir: Alternative antiviral option
- Vaccinia Immune Globulin (VIG): For severe complications
:max_bytes(150000):strip_icc()/scarlet-fever-treatment-770658_final-36a9d22aa54240478fd6633bc401ee73.png)
Current Outlook and Global Status
As of 2025, mpox remains a global health concern with ongoing surveillance and response efforts. The World Health Organization continues to monitor outbreaks, particularly the emergence of Clade Ib in Central Africa.
Global Statistics
- Over 100,000 cases reported globally since 2022
- Mortality rate varies by clade: 0.16% (Clade II) to 4.9% (Clade I)
- Endemic in 13 African countries
- Ongoing transmission in multiple continents
Public Health Response
International efforts focus on:
- Strengthening surveillance systems
- Improving vaccine access in affected regions
- Enhancing diagnostic capabilities
- Reducing stigma and discrimination
Frequently Asked Questions About Mpox
Is mpox deadly?
Most people recover completely from mpox. The fatality rate varies by viral clade, with Clade II having a very low mortality rate (0.16%) while Clade I can be more severe (up to 4.9% mortality).
How long does mpox last?
Mpox symptoms typically last 2-4 weeks. People remain infectious until all lesions have healed and new skin has formed underneath.
Can mpox be prevented?
Yes, mpox can be prevented through vaccination (for high-risk individuals), avoiding close contact with infected people, practicing good hygiene, and using barrier protection during sexual activity.
Who should get vaccinated against mpox?
Vaccination is recommended for healthcare workers, laboratory personnel, people with multiple sexual partners, and those with recent high-risk exposures to mpox.
How is mpox different from smallpox?
While both are caused by orthopoxviruses, mpox is generally less severe than smallpox. Mpox also causes swollen lymph nodes, which smallpox typically does not.
Can pets get mpox?
Yes, some animals can become infected with mpox. Pet owners should avoid contact with their pets if they have mpox and seek veterinary care if pets show symptoms.
Conclusion
Mpox remains an important public health challenge requiring continued vigilance and coordinated response efforts. Understanding the symptoms, transmission routes, and prevention strategies empowers individuals and communities to protect themselves and others. While most cases resolve without complications, early recognition and appropriate medical care are essential for optimal outcomes.
Stay informed about mpox developments through reliable health authorities like the CDC and WHO, and consult healthcare providers for personalized advice regarding vaccination and prevention strategies. With proper knowledge and preventive measures, we can continue to control mpox transmission and protect public health.